The idea to ‘flatten the curve'
The work of U-M historian and pediatrician Howard Markel, the director of U-M’s Center for the History of Medicine, helped inform a key response to the COVID-19 virus: “flattening the curve” or minimizing the number of infections by using non-pharmaceutical interventions (school closings, banning large events, wearing masks, etc.) until an effective treatment can be found.
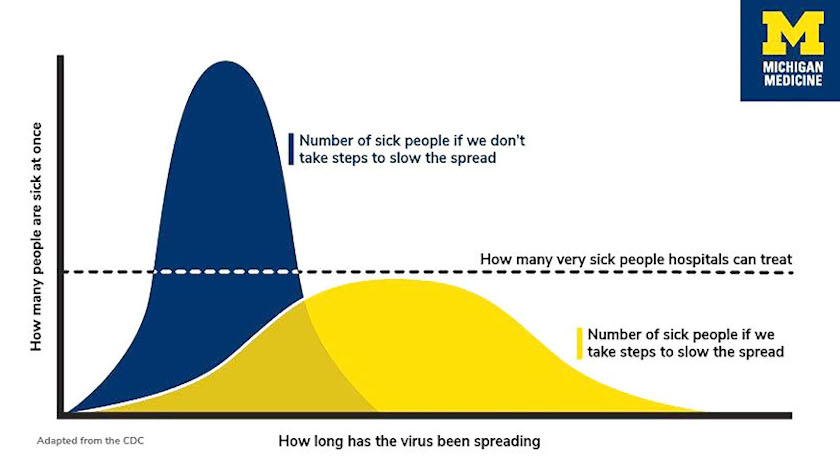
Markel and his colleagues studied the effects of efforts to stop the spread of the 1918 flu pandemic and the 2009 H1N1 flu epidemic. They found if individuals and communities took steps to slow the virus' spread, the number of cases could stretch out across a longer period of time. As the curve shows, the goal is to keep the number of cases at any given time below the dotted line of the capacity of our nation’s health care system so they can help everyone who’s very sick.
“If you don’t have as many cases coming to the hospitals and clinics at once, it can actually lower the number of total deaths from the virus and from other causes,” Markel explained. “And, importantly, it buys us time for university and government scientists, and industry, to create new therapies, medications and potentially a vaccine.”
Using these findings, the U.S. Centers for Disease Control and Prevention incorporated recommendations on how to “flatten the curve” in a 108-page primer titled “Interim Pre-pandemic Planning Guidance: Community Strategy for Pandemic Influenza Mitigation in the United States.” When the coronavirus started spreading globally, the CDC’s plan came off the shelf — and the phrase “flatten the curve” became a household term.
